Search
- Page Path
- HOME > Search
Research Articles
- [English]
- Sex differences in the association between Korean Healthy Eating Index and type 2 diabetes mellitus in Korean adults: a prospective cohort study
- Yeeun Park, Minji Kim, Kyong Park
- Korean J Community Nutr 2025;30(5):331-340. Published online October 31, 2025
- DOI: https://doi.org/10.5720/kjcn.2025.00227

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Objectives
Dietary quality is a modifiable determinant of type 2 diabetes mellitus (T2DM). However, evidence on the Korean Healthy Eating Index (KHEI) and sex-specific differences in its association with T2DM risk remains limited. This study is to examine the longitudinal association between KHEI and incident T2DM in Korean adults, with a focus on potential sex differences.
Methods
We analyzed 56,000 adults (37,684 women and 18,316 men) from the Health Examinee cohort of the Korean Genome and Epidemiology Study. Dietary intake was assessed using a validated semi-quantitative food frequency questionnaire, and KHEI scores were constructed based on national guidelines. Incident T2DM was defined using physician diagnosis, treatment history, or biochemical criteria. Cox proportional hazards models and restricted cubic spline analyses were applied to evaluate associations, with adjustments for demographic, lifestyle, and clinical covariates.
Results
Over a median follow-up of 4.2 years, 2,252 women and 1,776 men developed T2DM. Women in the highest quartile of KHEI had a 18% lower risk of T2DM compared with those in the lowest quartile (hazard ratio [HR]: 0.82, 95% confidence interval [CI]: 0.71–0.93; P for trend = 0.007). In men, no significant association was observed (HR: 1.11, 95% CI: 0.95–1.29). The interaction by sex was statistically significant (P for interaction < 0.05). Spline analyses indicated a linear inverse association between KHEI and T2DM risk in women, whereas no trend was evident in men.
Conclusion
Higher diet quality, as measured by the KHEI, was associated with a reduced risk of T2DM in women but not in men, suggesting sex-specific effects of dietary patterns on diabetes prevention. These findings highlight the need for tailored nutritional strategies that consider biological and behavioral differences between women and men in Korea.
- 257 View
- 10 Download

- [English]
- Comparison of clinical characteristics and dietary intakes according to phenotypes of type 2 diabetes mellitus in South Korea: a cross-sectional study
- Mi-Jin Kim, Ji-Sook Park, Sung-Rae Cho, Daeung Yu, Jung-Eun Yim
- Korean J Community Nutr 2025;30(2):127-139. Published online April 29, 2025
- DOI: https://doi.org/10.5720/kjcn.2025.00059
-
 Abstract
Abstract
 PDF
PDF - Objectives
Clinical nutrition treatment is the central part of diabetes management, such as prevention, treatment, and self-management of diabetes, and personalized clinical nutrition treatment, which enables improvement in patients with type 2 diabetes mellitus (T2DM). Our study aimed to contribute to the improvement of appropriate nutrition management in personalized treatment for obese and non-obese diabetes patients.
Methods
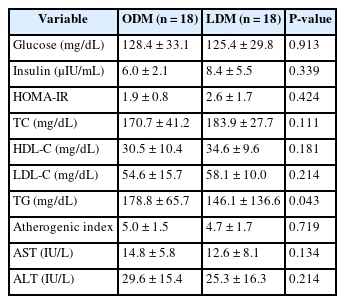
T2DM patients were recruited as participants, and 36 final participants were assigned to the lean diabetes mellitus group (LDM; body mass index [BMI] < 25 kg/m2) and the obese diabetes mellitus group (ODM; BMI ≥ 25 kg/m2). We assessed the dietary intakes, body composition, dietary habits, the Korean version of obesity-related quality of life, and biochemical indices.
Results
According to the phenotype’s comparison, the ODM group had a high prevalence of T2DM complications and hypertension, had a dietary habit of less than 10 minutes of mealtime duration and preferred fast food intake, and had a low obesity-related quality of life. However, the LDM group had a high choice of Korean dishes at the time of eating out and a high intake of vitamin C, and iodine because of the intake of vegetables and seaweeds.
Conclusion
We observed differences in diet, nutrient intake, and clinical characteristics according to the phenotype of T2DM patients. In particular, obese diabetes patients have an increased risk of cardiovascular diseases, bad dietary habits, and low obesity-related quality of life. Therefore, personalized nutrition treatment is needed in consideration of the risk of cardiovascular disease and dietary habits for patients in the ODM group, as well as determining the energy requirements of Korean patients with T2DM.
- 1,361 View
- 31 Download

- [English]
- Effects of a multi-component program based on partially hydrolyzed guar gum (Sunfiber®) on glycemic control in South Korea: a single-arm, pre-post comparison pilot clinical trial
- Hyoung Su Park, A-Hyun Jeong, Hyejung Hong, Hana Jang, Hye-Jin Kim
- Korean J Community Nutr 2025;30(1):40-52. Published online February 28, 2025
- DOI: https://doi.org/10.5720/kjcn.2024.00276
- Correction in: Korean J Community Nutr 2025;30(2):173

-
 Abstract
Abstract
 PDF
PDF - Objectives
The aim of this study was to assess the impact of a multi-component program, including partially hydrolyzed guar gum (PHGG, Sunfiber®) supplementation, on glycemic control, gut health, and nutritional status to support diabetes prevention and management among Korean adults.
Methods
A single-arm trial was conducted with 29 adults (aged 20-55 years) with fasting plasma glucose (FPG) ≥ 100 mg/dL. Over a six-week period, participants engaged in a multi-component program that incorporated the supplementation of PHGG (Sunfiber®, 12.5 g/day), weekly nutritional coaching, and the use of continuous glucose monitoring devices. The program’s effectiveness was evaluated by measuring FPG and glycated hemoglobin (HbA1c) levels through blood tests conducted before and after the intervention. Improvements in gut health were gauged using the Korean Gut Quotient Measurement Scales, while enhancements in nutritional status were assessed using the Nutrition Quotient (NQ) and surveys that evaluated improvements in gut health and nutritional status.
Results
Participants’ average age was 43.89 years, with approximately 80% being male. Most participants (about 75%) were classified as overweight or obese. After six-weeks, 17 participants who adhered closely to the program (meeting certification criteria) exhibited significant reductions in key blood glucose markers. FPG levels decreased from 113.06 ± 23.16 mg/dL to 106.24 ± 16.33 mg/dL (P < 0.05), and HbA1c levels decreased from 6.08% ± 0.81% to 5.87% ± 0.53% (P < 0.05). The NQ evaluation revealed significant increases in comprehensive nutrition scores, and in the balance and practice domain scores for all participants (P < 0.05). Furthermore, in the gut health survey, approximately 82.1% of all participants reported experiencing positive changes.
Conclusion
Among adults with elevated FPG levels, a multi-component intervention program that included PHGG (Sunfiber®) supplementation, structured dietary management, and the use of health-monitoring devices showed significant benefits in improving glycemic control, overall nutritional status, and gut health. Trial Registration: Clinical Research Information Service Identifier: KCT0010049.
- 6,195 View
- 41 Download

- [Korean]
- Impact of a public health center nutrition education program on patients with type 2 diabetes in a primary care-based chronic disease management project: a pilot intervention study
- Haerim Yang, Yoo Kyoung Park, Ji-hyun Lee, Hee-Sook Lim, Heejoon Baek, Hyejin Lee, Haeran Park, Pyunghwa Lee, Jooyoun Chung, Won Gyoung Kim
- Korean J Community Nutr 2024;29(6):492-503. Published online December 31, 2024
- DOI: https://doi.org/10.5720/kjcn.2024.00018
-
 Abstract
Abstract
 PDF
PDF - Objectives
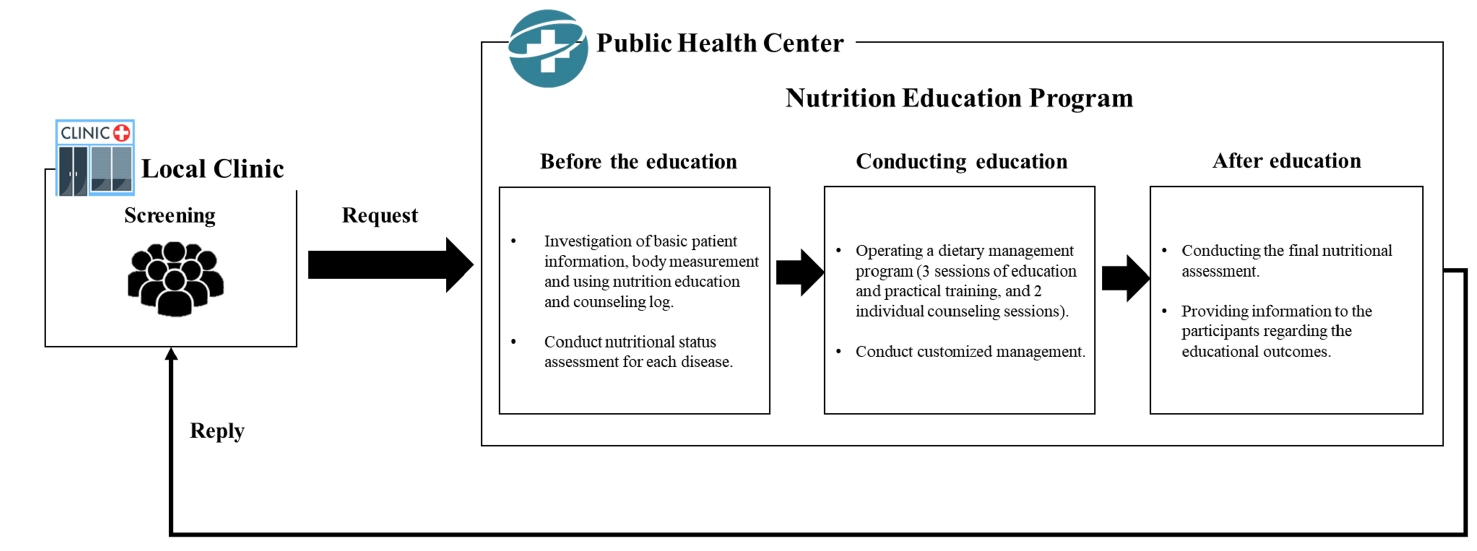
We investigated the impact of an advanced “Nutrition Education Program” on patients with Diabetes mellitus, type 2 from public health centers enrolled in a primary health care-based chronic disease management project. This 12-week dietary management program was developed by the Korea Health Promotion and Development Institute. We assessed if this program improved glycemic control and other health indicators through dietary and nutritional improvements.
Methods
Seventeen patients with Diabetes mellitus type 2 were enrolled in the “Nutrition Education Program.” These patients were referred to public health centers for lifestyle management based on physician assessments at local clinics that were participating in a pilot project on primary health care-based chronic disease management. The participants attended the program comprising face-to-face basic, in-depth, and practical training sessions at the health center during the third, fifth, and seventh weeks, respectively. Anthropometric measurements, body composition analysis, blood biochemical characteristics, nutritional knowledge, and self-efficacy evaluation were performed before and after the program. Data were analyzed using SPSS ver. 28.0.
Results
The mean age of the participants was 62 years, and most participants were female (14, 82.4%). No significant changes in patients’ anthropometric measurements or body composition were observed after the training. However, significant reductions were observed in the blood biochemical characteristics, including glycated hemoglobin, total cholesterol, and low-density lipoprotein levels. Additionally, patients’ nutritional knowledge and self-efficacy scores increased significantly.
Conclusions
The “Nutrition Education Program” helped in improving glycemic control and other health indicators in patients with Diabetes mellitus type 2. Further research is required to objectively confirm the long-term and sustained effects of the program in a controlled study. Trial Registration Clinical Research Information Service Identifier: KCT0010010
- 1,823 View
- 74 Download

- [English]
- Health-related quality of life and nutrient intake of the elderly with type 2 diabetes according to comorbidity burden: a cross-sectional study
- Yejung Choi, Kyong Park
- Korean J Community Nutr 2024;29(5):418-430. Published online October 31, 2024
- DOI: https://doi.org/10.5720/kjcn.2024.00014
-
 Abstract
Abstract
 PDF
PDF - Objectives
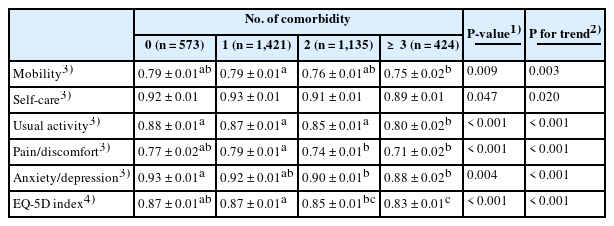
This study aimed to explore the cross-sectional association between health-related quality of life (HRQoL) according to the number of comorbidities in older adults with type 2 diabetes mellitus (T2DM) using the Euro Quality of Life-5 Dimensions (EQ-5D) index. Methods: This study included 3,553 participants aged ≥ 65 years from the 2008–2020 Korea National Health and Nutrition Examination Survey. Dietary data were collected through 24-hour recall interviews by trained researchers, and demographic and lifestyle information via self-administered questionnaires. HRQoL was measured using a modified EQ-5D scale. Multivariable linear regression analyzed the associations between EQ-5D scores, nutrients and comorbidity, controlling for sociodemographic and health variables. Results: Most participants reported ‘no problems’ in the EQ-5D scores, although approximately 17% to 47% of participants reported ‘some problems’ or ‘extreme problems,’ depending on the dimension. As comorbidities increased, significant declines were observed across all dimensions, particularly in mobility, usual activities, pain/discomfort, and anxiety/ depression. Nutrient intake analysis revealed that participants with three or more comorbidities consumed less carbohydrates, but more fat. Conclusion: Our findings demonstrate that among older adults with T2DM, a higher number of comorbidities is associated with decreased HRQoL. Additionally, there are differences in nutrient intake patterns among those with more comorbidities, specifically decreased carbohydrate intake and increased fat intake. These results emphasize the need for comprehensive and tailored management strategies that consider both diabetes and the co-occurring health conditions. By addressing the complex healthcare needs of individuals with multiple comorbidities, it is possible to enhance their HRQoL and overall well-being.
- 1,667 View
- 28 Download

- [English]
- Sex differences in health-related quality of life among older Korean adults with type 2 diabetes mellitus: a cross-sectional study
- Hyeonji Jeong, Kyong Park
- Korean J Community Nutr 2024;29(4):336-347. Published online August 31, 2024
- DOI: https://doi.org/10.5720/kjcn.2024.00003
-
 Abstract
Abstract
 PDF
PDF - Objectives
This cross-sectional study examined sex differences in Health-Related Quality of Life (HRQoL) among seniors with Type 2 Diabetes Mellitus (T2DM).
Methods
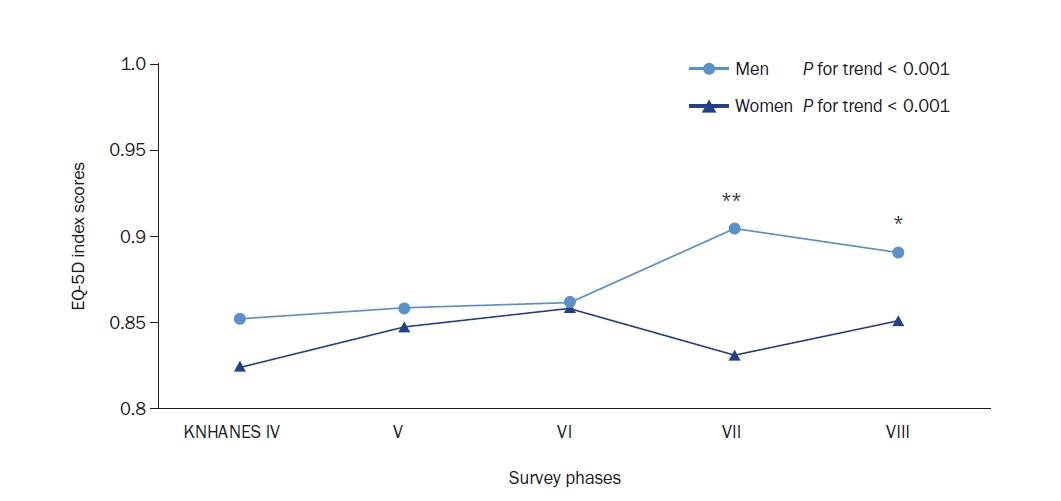
Data from the Korea National Health and Nutrition Examination Survey (2008–2020) were analyzed. The EuroQol-5 Dimensions (EQ-5D), a measure of HRQoL, was used. It comprises five dimensions: mobility, self-care, usual activity, pain/discomfort, and anxiety/depression, each with three levels.
Results
Analysis of 3,826 older adults with T2DM showed a significant increasing trend in the EQ-5D Index from the 4th survey phase onwards (P for trend < 0.001 for both men and women). Men consistently reported higher EQ-5D levels than women across all survey years. Women’s EQ-5D levels remained lower than men’s, maintaining a decade-old disparity (P < 0.05). Men scored significantly higher (P < 0.05) in most EQ-5D domains, except for self-care and anxiety/depression, resulting in a higher total EQ-5D Index (P = 0.001). Increased comorbidities were strongly associated with lower EQ-5D levels in both sexes. Additionally, there was a negative correlation between the EQ-5D Index and refined grain intake for both sexes (P for trend < 0.001), with high-EQ-5D groups consuming fewer refined grains. Women in the high-EQ-5D group consumed more nuts, vegetables, and meat compared to men (P for trend < 0.05).
Conclusions
Our study highlights the sex disparities in HRQoL among older adults with T2DM. The findings suggest the need for tailored treatment guidelines aimed at improving the HRQoL of elderly T2DM patients, with a focus on their sex-specific characteristics. Implementing these tailored guidelines could enhance the HRQoL of older women with T2DM and promote more equitable healthcare outcomes. This underscores the importance of considering sex differences to comprehensively improve the well-being of this population. -
Citations
Citations to this article as recorded by- Understanding Gender Disparities in Quality of Life Among Patients With Type 2 Diabetes in Ethiopia: An Institutional‐Based Study
Enguday Demeke Gebeyaw, Girma Deshimo Lema
Lifestyle Medicine.2025;[Epub] CrossRef
- Understanding Gender Disparities in Quality of Life Among Patients With Type 2 Diabetes in Ethiopia: An Institutional‐Based Study
- 2,078 View
- 39 Download
- 1 Crossref


 KSCN
KSCN

 First
First Prev
Prev



