Abstract
-
Objectives
- Dietary quality is a modifiable determinant of type 2 diabetes mellitus (T2DM). However, evidence on the Korean Healthy Eating Index (KHEI) and sex-specific differences in its association with T2DM risk remains limited. This study is to examine the longitudinal association between KHEI and incident T2DM in Korean adults, with a focus on potential sex differences.
-
Methods
- We analyzed 56,000 adults (37,684 women and 18,316 men) from the Health Examinee cohort of the Korean Genome and Epidemiology Study. Dietary intake was assessed using a validated semi-quantitative food frequency questionnaire, and KHEI scores were constructed based on national guidelines. Incident T2DM was defined using physician diagnosis, treatment history, or biochemical criteria. Cox proportional hazards models and restricted cubic spline analyses were applied to evaluate associations, with adjustments for demographic, lifestyle, and clinical covariates.
-
Results
- Over a median follow-up of 4.2 years, 2,252 women and 1,776 men developed T2DM. Women in the highest quartile of KHEI had a 18% lower risk of T2DM compared with those in the lowest quartile (hazard ratio [HR]: 0.82, 95% confidence interval [CI]: 0.71–0.93; P for trend = 0.007). In men, no significant association was observed (HR: 1.11, 95% CI: 0.95–1.29). The interaction by sex was statistically significant (P for interaction < 0.05). Spline analyses indicated a linear inverse association between KHEI and T2DM risk in women, whereas no trend was evident in men.
-
Conclusion
- Higher diet quality, as measured by the KHEI, was associated with a reduced risk of T2DM in women but not in men, suggesting sex-specific effects of dietary patterns on diabetes prevention. These findings highlight the need for tailored nutritional strategies that consider biological and behavioral differences between women and men in Korea.
-
Keywords: diet, healthy; diabetes mellitus, type 2; sex factors; cohort studies
INTRODUCTION
Diabetes mellitus poses a global health crisis. It causes chronic hyperglycemia and drives complications, early mortality, poor quality of life, and mounting socioeconomic costs [1, 2]. By 2050, over 800 million adults may be affected globally, according to the International Diabetes Federation [1].
Diet quality is a key modifiable risk factor for type 2 diabetes mellitus (T2DM) [3-5]. Composite diet indexes capture holistic eating patterns more effectively than isolated nutrient metrics [6-10]. The Korean Healthy Eating Index (KHEI), developed by the Korea Disease Control and Prevention Agency, was constructed using analyses of Korea National Health and Nutrition Examination Survey (KNHANES) data and reflects adherence to national guidelines via components encompassing adequacy, moderation, and energy balance [6].
Emerging evidence links higher KHEI scores to reduced healthcare costs and metabolic risk in Koreans. A nationwide study found that better diet quality was associated with lower inpatient and total medical expenditures, while another report showed that low KHEI scores were linked to higher chronic disease burden in middle-aged single-person households [8, 11]. These findings highlight KHEI’s potential to inform both clinical and public health strategies.
Diet influences T2DM risk through metabolic pathways that vary by sex. Women generally exhibit greater insulin sensitivity, partly due to estrogen-driven mechanisms that enhance glucose homeostasis [12, 13]. In Korea, metabolic syndrome prevalence rose markedly in men (24.5% → 36.8%) from 2007 to 2022, while it declined in women (20.6% → 19.5%) [11]. Moreover, risk factors for metabolic syndrome differ by sex: alcohol consumption is a major driver in men, whereas behavioral and socioeconomic factors are more influential in women [14]. Recent studies also show that higher Korean Healthy Diet Scores are associated with lower prevalence of metabolic syndrome and its components [15]. These observations suggest that differences in metabolic profiles and risk factors between men and women may shape how diet quality influences diabetes risk. In particular, sex-specific pathways observed for metabolic syndrome provide a biological rationale to expect similar differences in the association between KHEI and incident T2DM.
Despite these insights, few longitudinal cohort studies in Korea have investigated whether diet quality, as measured by KHEI, differentially predicts T2DM risk in men and women. To address this gap, we analyzed the prospective association between KHEI and incident T2DM using the Health Examinee (HEXA) cohort of the Korean Genome and Epidemiology Study (KoGES). We hypothesized that higher KHEI scores would be associated with a lower risk of T2DM, with stronger inverse associations expected among women compared with men.
METHODS
Ethics statement
All participants provided written informed consent after trained investigators explained the purpose and procedures of KoGES. The study protocol was approved by the Institutional Review Boards of the Korea Disease Control and Prevention Agency and Yeungnam University (IRB No. 7002016-E-2016-003).
1. Study design
This is a prospective cohort study. It was described according to the Strengthening the Reporting of Observational Studies in Epidemiology statement (https://www.strobe-statement.org/).
2. Study participants
This study used data from the HEXA cohort of the KoGES [16, 17]. The HEXA cohort was selected for its comprehensive data collection, standardized protocols, and continuous quality control through investigator training and monitoring, ensuring high reliability [16, 17]. Designed to investigate environmental and genetic risk factors for major chronic diseases, the HEXA survey targeted men and women aged 40–79 years from urban health examination centers across Korea. The baseline survey was conducted between 2004 and 2013, and the first follow-up survey between 2012 and 2016 at 17 of the original 39 institutions [16, 17].
A total of 173,200 individuals participated in the baseline survey, of whom 65,610 completed the first follow-up. For the present analysis, we excluded participants with implausible energy intake (< 500 or > 5,000 kcal/day, n = 3,899) [18], pre-existing T2DM at baseline (n = 11,295), a history of cardiovascular disease or cancer at baseline (n = 9,608), or no follow-up participation (n = 92,398). The final analytic sample included 56,000 adults.
3. Demographic and lifestyle information
At baseline, trained investigators collected detailed demographic and lifestyle data [19]. Information included sex, age, and marital status (married, including cohabiting, vs. non-married, including never married, separated, divorced, and widowed). Educational attainment was classified as below high school or high school and above. Smoking status was categorized as never, former, or current smoker, and alcohol consumption as current drinker or non-drinker (including past drinkers).
Household income was calculated as the total monthly income from all sources and categorized into 4 groups: < 1,000,000 Korean won (KRW), 1,000,000–1,999,999 KRW, 2,000,000–3,999,999 KRW, and ≥ 4,000,000 KRW. Physical activity was evaluated based on a KoGES survey question regarding regular engagement in exercise intense enough to cause sweating. Information on family history of T2DM and prior diagnoses of hypertension or dyslipidemia was collected. Trained staff measured height and weight following standardized protocols, and body mass index (BMI) was calculated as weight (kg)/height (m2) [20].
4. Dietary information and Korean Healthy Eating Index
Dietary intake was assessed using a validated semi-quantitative food frequency questionnaire (SQFFQ) consisting of 106 food items, previously evaluated for reproducibility and validity in Korean populations [21]. Participants reported their habitual dietary intake over the past year. In cases of recent dietary changes, responses were instructed to reflect their usual diet prior to the change. To improve accuracy, the SQFFQ included portion size photographs and seasonally adjusted food items.
The KHEI was constructed from SQFFQ data using a framework developed from analyses of the KNHANES data [6]. Several modifications were made to tailor the index to KoGES data and to avoid redundancy. Specifically, the original component “having breakfast” was replaced with “number of meals per day” to better reflect dietary regularity; kimchi and other pickled vegetables were excluded from the total vegetable intake category given their high sodium content and established association with cardiometabolic risk [22]; and the “milk and milk products” category was refined to exclude ice cream. The final KHEI included 12 components grouped into adequacy (n = 6), moderation (n = 3), and energy balance (n = 3) domains (Supplementary Table 1).
Dietary intakes were converted into servings per day using standardized conversion factors, with portion sizes defined by the 2020 Korean Dietary Reference Intakes [23]. For moderation components, intakes of saturated fat sources (e.g., pork belly, cream, butter/margarine, cakes, instant noodles) and sweets/beverages (e.g., soda, confectionery, sweetened drinks) were scored inversely, with intake levels divided into 11 quantiles to capture graded variation. Sodium intake was scored from 0 to 10 based on thresholds from ≤ 2,000 mg/day to > 6,500 mg/day. Energy balance was evaluated by calculating the percentage of daily energy from carbohydrates (optimal: 55%–65%) and fats (optimal: 15%–30%), as well as the ratio of total energy intake to estimated energy requirement (optimal: 75%–125%). The resulting KHEI had a total score range of 0 to 90 points, with higher scores indicating closer adherence to dietary guidelines and overall better diet quality.
5. Definition of T2DM diagnosis
Information on disease history and medication use was collected by trained investigators. T2DM was defined according to the Korean Diabetes Association [24]: (1) physician diagnosis, (2) current or past treatment with medication or insulin, (3) fasting plasma glucose ≥ 126 mg/dL, or (4) hemoglobin A1c ≥ 6.5%.
6. Statistical analysis
Participant characteristics across KHEI quartiles were compared using chi-square tests for categorical variables and generalized linear regression for continuous variables. The association between KHEI and incident T2DM was evaluated with Cox proportional hazards regression, and results were expressed as hazard ratios (HRs) and 95% confidence intervals (CIs). Follow-up time was calculated from the baseline survey date to the date of T2DM diagnosis, or to the last follow-up date for censored cases.
Potential confounding variables were identified through literature review and preliminary analyses, focusing on demographic, socioeconomic, lifestyle, and clinical factors known to influence both diet quality and T2DM risk [13, 24, 25]. In addition, potential effect modifiers were evaluated by introducing multiplicative interaction terms between KHEI and candidate variables. Sex emerged as a significant effect modifier, and therefore all analyses were stratified by men and women. The statistical significance of interaction terms (P for interaction) was assessed using Wald tests within the Cox regression models.
Based on this identification process, 3 regression models were constructed. Model 1 was adjusted for age. Model 2 was additionally adjusted for education, household income, smoking status, alcohol consumption, physical activity, BMI, marital status, and total energy intake. Model 3 was further adjusted for hypertension, dyslipidemia, and family history of T2DM. The dose–response relationship between KHEI scores and T2DM risk was examined using restricted cubic spline regression with 4 knots placed at the 5th, 35th, 65th, and 95th percentiles of the KHEI distribution. The median KHEI score was set as the reference value. We confirmed that sensitivity analyses using alternative knot specifications yielded similar results. Models were adjusted for the same covariates as Model 3. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc.), and the threshold for statistical significance was set at α = 0.05.
RESULTS
The median follow-up period was 4.2 years. During this time, the incidence rate of T2DM was 11.99 per 1,000 person-years in women and 19.32 per 1,000 person-years in men. Table 1 presents the baseline demographic and lifestyle characteristics of the participants stratified by sex. The median KHEI scores were 54.01 in women and 50.16 in men. The average age was 52.42 years in women and 54.36 years in men. The proportion of participants in the highest household income group was 25.04% among women and 28.59% among men. A high school education or higher was reported by 65.31% of women and 79.73% of men. In women, 97.14% were non-smokers and 69.29% were non-drinkers, compared with 29.78% and 26.24% in men, respectively. Regular physical activity was reported by 53.44% of women and 59.09% of men. The mean BMI and total energy intake were 23.52 kg/m2 and 1,706.30 kcal/day in women, and 24.38 kg/m2 and 1,855.04 kcal/day in men. In addition, the prevalence of hypertension, dyslipidemia, being married, and a family history of T2DM was 14.95%, 8.53%, 97.26%, and 13.82% in women, compared with 20.66%, 9.25%, 97.25%, and 10.67% in men.
Table 2 presents the longitudinal association between KHEI quartiles and incident T2DM stratified by sex, as the interaction by sex was statistically significant (P for interaction < 0.05). Among women, those in the highest quartile had a 21% lower risk of T2DM compared with those in the lowest quartile (HR = 0.79, 95% CI: 0.70–0.89) in age-adjusted Model 1. This association remained significant after additional adjustment for socioeconomic, lifestyle, and dietary factors in Model 2 (HR = 0.83, 95% CI: 0.73–0.95), and after further adjustment for clinical factors in Model 3 (HR = 0.82, 95% CI: 0.71–0.93). A significant linear trend was observed across quartiles in all models (P for trend < 0.001, 0.016, and 0.007, respectively). When analyzed as a continuous variable, each one-point increase in KHEI score was associated with lower risk of T2DM (HR = 0.99, 95% CI: 0.98–0.99; Model 3, data not shown). In contrast, no significant associations were observed in men. The HRs for the highest versus lowest quartile were 1.02 (95% CI: 0.89–1.16) in Model 1, 1.13 (95% CI: 0.97–1.31) in Model 2, and 1.11 (95% CI: 0.95–1.29) in Model 3. The continuous analysis similarly showed no association (HR = 1.00, 95% CI: 0.99–1.01; Model 3, data not shown), with no evidence of a linear trend across quartiles.
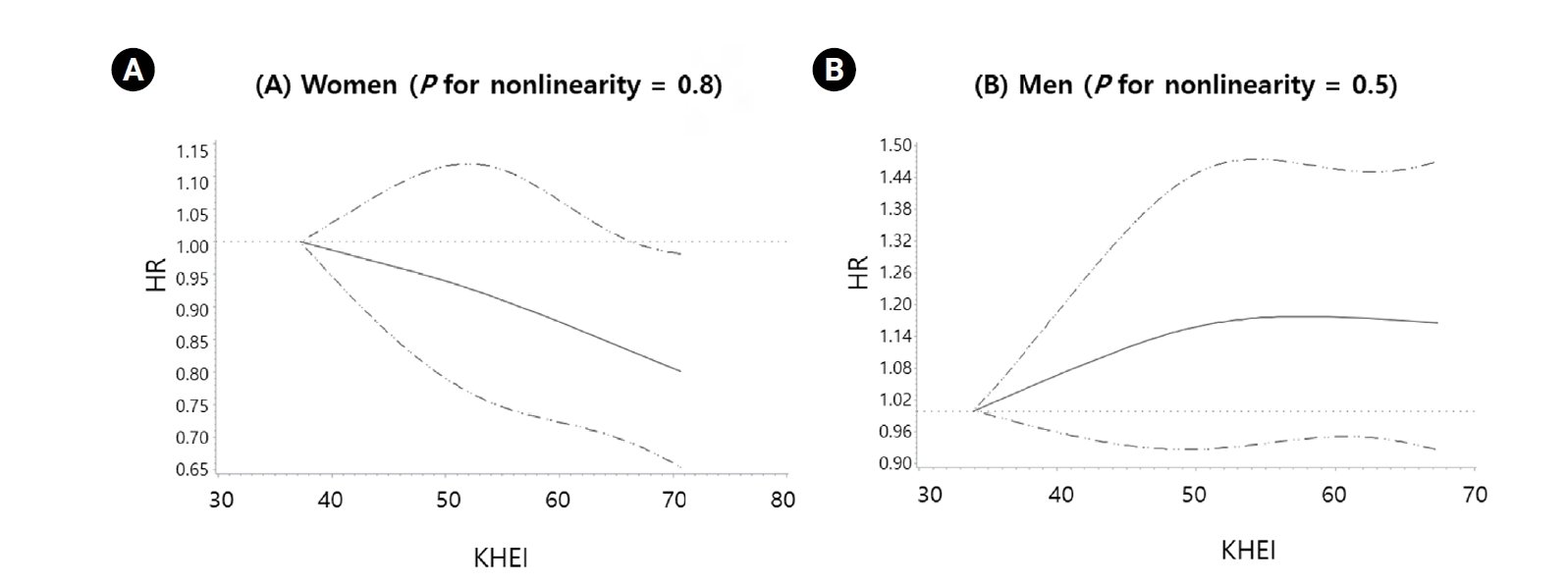
Fig. 1 illustrates restricted cubic spline curves for the association between KHEI scores and incident T2DM. After adjustment for the same covariates as in Model 3 of Table 2, no evidence of nonlinearity was observed in either sex (P for nonlinearity = 0.8 in women; 0.5 in men). In women, however, a clear linear inverse association was evident, with T2DM risk decreasing steadily as KHEI scores increased. By contrast, no such association was observed in men.
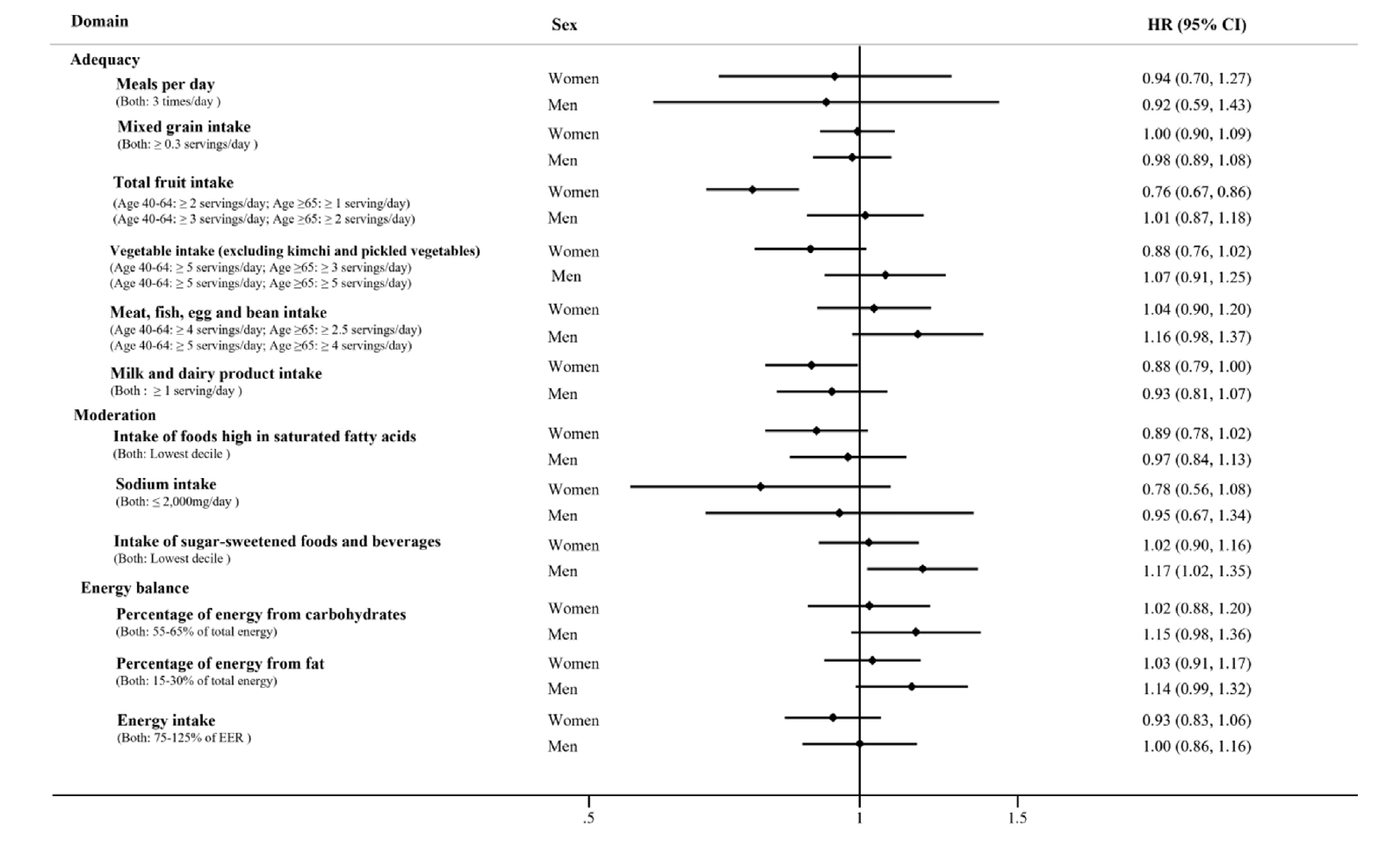
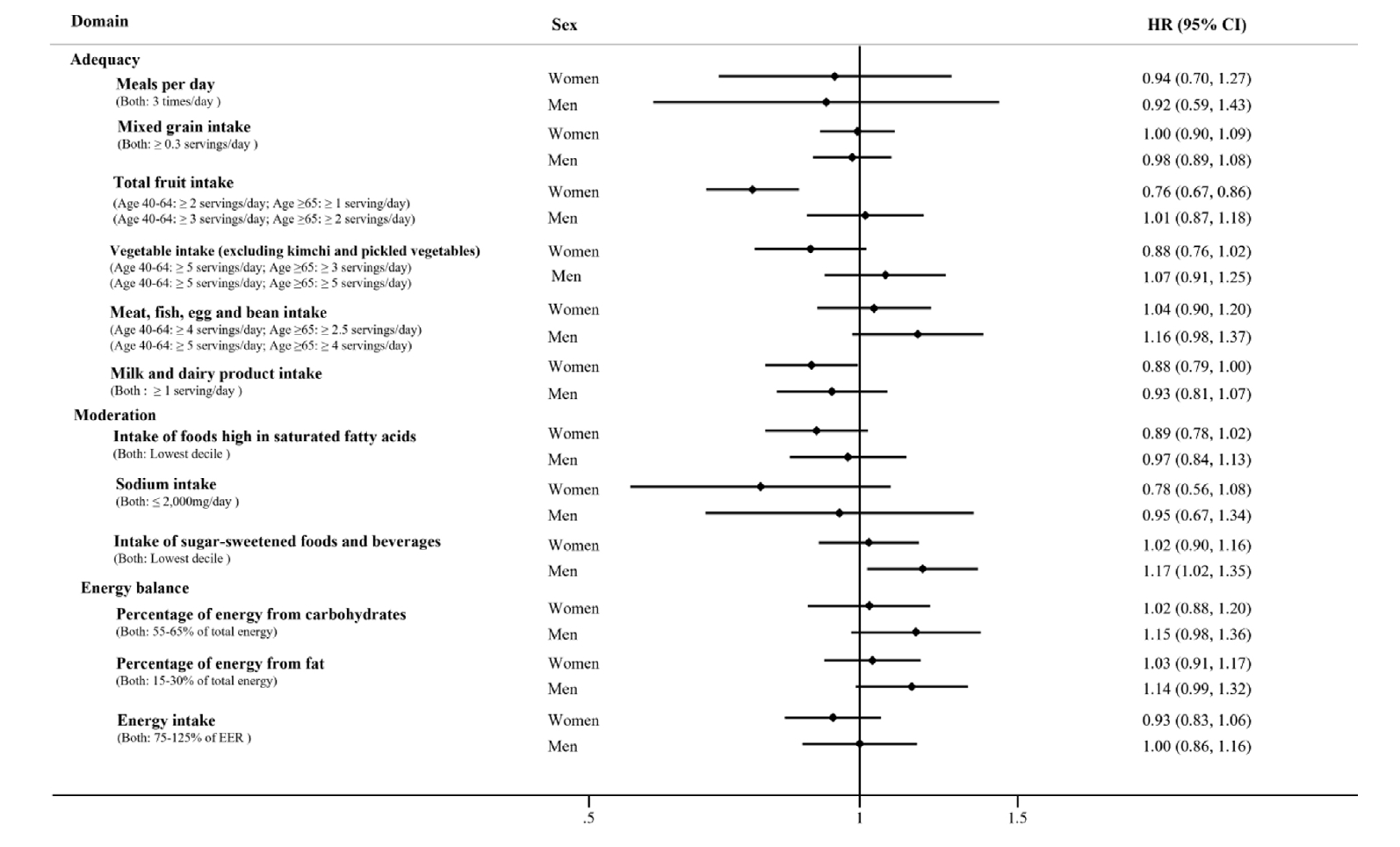
Fig. 2 presents multivariable-adjusted HRs and 95% CIs for T2DM according to the individual components of the KHEI, grouped into adequacy, moderation, and energy balance domains. Across all components, women consistently exhibited lower HRs than men, indicating stronger protective associations between healthier dietary patterns and reduced diabetes risk. The only exceptions were “meals per day” and “mixed grain intake,” where men showed slightly lower HRs than women, although the differences were minimal and the overall patterns were similar between sexes.
DISCUSSION
In this large prospective cohort, higher KHEI scores were associated with a significantly lower risk of T2DM in women, but not in men. This finding was consistent in dose–response analyses, which showed a linear inverse relationship between diet quality and T2DM risk in women. These results highlight the relevance of dietary quality as a modifiable factor in diabetes prevention and underscore potential sex-specific differences in metabolic responses to diet.
Our findings are consistent with prior studies showing that healthy dietary patterns, such as the Mediterranean diet, are associated with reduced diabetes risk [26-29], and extend this evidence by demonstrating a stronger association in women. Importantly, by applying the KHEI—a tool specifically adapted to Korean dietary practices—our study provides culturally relevant evidence that extends beyond global diet indices. This addresses a critical gap in the literature by evaluating a localized dietary index within an Asian population and by examining sex-specific associations.
The observed protective effect of diet quality in women may be explained by several mechanisms. Diets rich in whole grains, fruits, and vegetables provide dietary fiber and polyphenols, which improve insulin sensitivity, reduce postprandial glycemia, and lower systemic inflammation [30-38]. Fiber fermentation promotes glucagon-like peptide-1 secretion, while polyphenols exert antioxidant and anti-inflammatory effects that mitigate β-cell dysfunction and insulin resistance [35, 37]. High-quality diets are also linked to lower adiposity and improved lipid profiles, both of which are central to diabetes prevention [24, 35, 39]. Together, these pathways offer a biological rationale for the observed inverse association between KHEI and T2DM in women.
The stronger association in women compared with men warrants further consideration. Women are more likely to adopt health-conscious behaviors and maintain dietary compliance, which may amplify the benefits of a high-quality diet [40]. Additionally, estrogen enhances insulin action and glucose homeostasis, providing further metabolic protection in women [41, 42]. By contrast, men’s dietary patterns may be more heavily influenced by alcohol consumption and other lifestyle factors, potentially attenuating the protective role of diet quality [14]. These observations suggest that sex-specific biological and behavioral factors jointly shape the relationship between diet quality and diabetes risk.
Analysis of individual KHEI components further supports this conclusion. Women exhibited lower HRs across nearly all components, with fruit intake showing the strongest protective association. Men showed slightly lower HRs only for mixed grain intake and the number of meals per day, though the differences compared with women were minimal. This pattern reinforces the conclusion that overall diet quality is particularly important for women, while isolated components may have limited effects in men. In addition, the HRs in men were consistently close to 1.0 with relatively narrow CIs, suggesting that limited statistical power is unlikely to explain the null association. Residual confounding is also unlikely to differ substantially by sex. Instead, the lower overall KHEI scores and weaker component-specific associations observed in men support the interpretation that diet quality exerts genuinely weaker protective effects in this group.
Another methodological consideration is that the KHEI used in this study was slightly modified to fit the KoGES data and the Korean dietary context. Replacing breakfast frequency with number of meals per day allowed a more comprehensive assessment of dietary regularity, while excluding kimchi and pickled vegetables from the vegetable component minimized potential misclassification due to their high sodium content. Refining the milk and dairy category by excluding ice cream also improved construct validity by removing foods high in added sugars and saturated fats. These modifications are unlikely to bias the results but rather enhance the relevance of the KHEI for evaluating T2DM risk in this population.
Limitations
Several limitations should be noted. First, despite adjusting for multiple confounders, residual confounding by unmeasured factors, including prior dietary history, cannot be ruled out. Second, the KHEI was derived from a SQFFQ. Although this tool is validated, the restricted food list and reliance on self-reported frequency data may have led to underestimation or misclassification of dietary intake. Third, because the KHEI was specifically developed for the Korean population, caution is required when generalizing these findings to populations with different dietary patterns. Fourth, the median follow-up period was relatively short, which limited the number of incident T2DM cases. Fifth, a substantial proportion of participants did not complete follow-up, raising the possibility of selection bias, although the large remaining sample still provided sufficient statistical power. Nevertheless, to our knowledge, this study is the first large-scale prospective investigation of KHEI and incident T2DM stratified by sex, and it provides novel insights into both the cultural and biological dimensions of diet–disease relationships.
Conclusion
Higher KHEI scores were associated with a lower risk of T2DM in women but not in men. These findings highlight the importance of overall diet quality in diabetes prevention, particularly among women, and underscore the need to consider sex-specific factors in nutritional research. Further studies in diverse populations are warranted to confirm these associations and to clarify the biological and behavioral mechanisms that may inform tailored dietary strategies and public health interventions.
NOTES
-
CONFLICT OF INTEREST
There are no financial or other issues that might lead to conflict of interest.
-
FUNDING
This research was funded by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (grant number: 2021R1A2C1007869). The funders had no role in the study design; collection, analyses, or interpretation of data; writing of the manuscript; or decision to publish the results.
-
ACKNOWLEDGEMENTS
Data were obtained from the Korean Genome and Epidemiology Study (KoGES; 4851-302), National Research Institute of Health, Korea Disease Control and Prevention Agency, Ministry for Health and Welfare, Republic of Korea.
-
DATA AVAILABILITY
The original data presented in the study are openly available in the Korean Genome and Epidemiology Study (KoGES) at https://www.nih.go.kr upon reasonable request and approval.
SUPPLEMENTARY MATERIALS
Fig. 1.Restricted cubic spline curves for the association between Korean Healthy Eating Index (KHEI) scores and incident type 2 diabetes mellitus (T2DM) in women (A, n = 37,684) and men (B, n = 18,316). Solid lines represent hazard ratios and dashed lines 95% confidence intervals. Models were adjusted for age, education, household income, smoking status, alcohol consumption, physical activity, body mass index, marital status, total energy intake, hypertension, dyslipidemia, and family history of T2DM. No evidence of nonlinearity was observed in either sex (P for nonlinearity = 0.8 for women; 0.5 for men). HR, hazard ratio
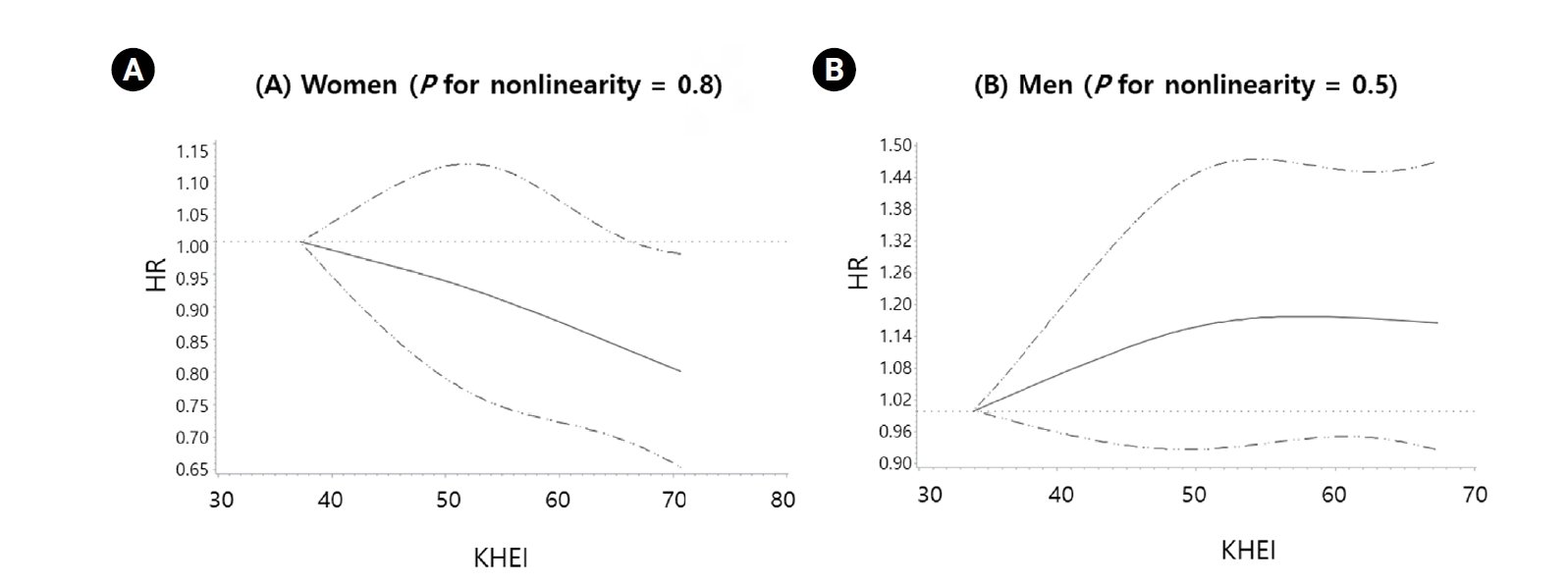
Fig. 2.Multivariable-adjusted hazard ratios (HR) (95% confidence intervals [CI]) for type 2 diabetes mellitus (T2DM) according to individual components of the Korean Healthy Eating Index, grouped into adequacy, moderation, and energy balance domains, stratified by sex. Models were adjusted for age, education, household income, smoking status, alcohol consumption, physical activity, body mass index, marital status, total energy intake, hypertension, dyslipidemia, and family history of T2DM. EER, estimated energy requirement.
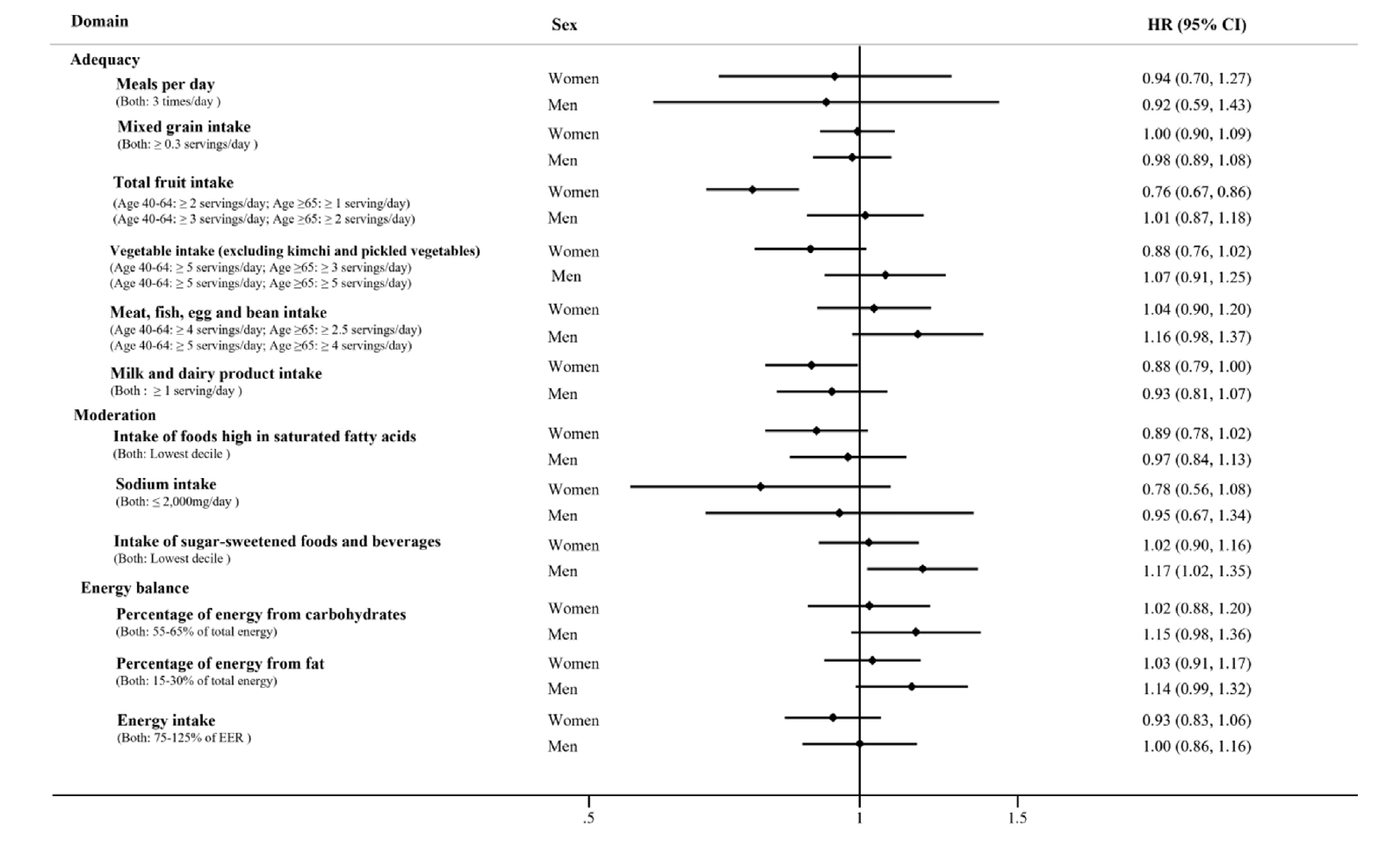
Table 1.Demographic and lifestyle characteristics of study participants by sex (n = 56,000)
|
Characteristics |
Men (n = 18,316) |
Women (n = 37,684) |
P-value1)
|
|
No. of participants |
18,316 |
37,684 |
|
|
Age (year) |
54.36 ± 0.06 |
52.42 ± 0.04 |
< 0.001 |
|
Household income |
|
|
< 0.001 |
|
Low |
1,219 (7.25) |
3,621 (10.83) |
|
|
Mid-low |
3,066 (18.24) |
6,750 (20.17) |
|
|
Mid-high |
7,720 (45.92) |
14,712 (43.96) |
|
|
High |
4,806 (28.59) |
8,380 (25.04) |
|
|
Education level |
|
|
< 0.001 |
|
< High school |
3,670 (20.27) |
12,916 (34.69) |
|
|
≥ High school |
14,434 (79.73) |
24,319 (65.31) |
|
|
Smoking status |
|
|
< 0.001 |
|
Non-smokers |
5,442 (29.78) |
36,433 (97.14) |
|
|
Former smokers |
7,703 (42.16) |
432 (1.15) |
|
|
Current smokers |
5,126 (28.06) |
643 (1.71) |
|
|
Alcohol consumption |
|
|
< 0.001 |
|
Non-drinkers |
4,790 (26.24) |
25,986 (69.29) |
|
|
Current drinkers |
13,463 (73.76) |
11,517 (30.71) |
|
|
Physical activity level2)
|
|
|
< 0.001 |
|
Inactive |
7,467 (40.91) |
17,492 (46.56) |
|
|
Active |
10,785 (59.09) |
20,073 (53.44) |
|
|
Body mass index (kg/m2) |
|
|
< 0.001 |
|
< 25 |
11,124 (60.77) |
27,542 (73.12) |
|
|
≥ 25 |
7,182 (39.23) |
10,125 (26.88) |
|
|
Total energy intake (kcal/day) |
1,855.04 ± 3.79 |
1,706.30 ± 2.71 |
< 0.001 |
|
Hypertension (Yes) |
3,784 (20.66) |
5,633 (14.95) |
< 0.001 |
|
Dyslipidemia (Yes) |
1,695 (9.25) |
3,215 (8.53) |
0.005 |
|
Marital status (Yes) |
17,387 (97.25) |
35,443 (97.26) |
0.958 |
|
Family history of type 2 diabetes mellitus (Yes) |
1,954 (10.67) |
5,209 (13.82) |
< 0.001 |
Table 2.Hazard ratios (95% confidence intervals) for incident type 2 diabetes mellitus according to quartiles of the Korean Healthy Eating Index (KHEI), stratified by sex (n = 56,000)
|
Quartiles of KHEI
|
P for trend |
|
Q1 |
Q2 |
Q3 |
Q4 |
|
Women (n = 37,684) |
|
|
|
|
|
|
No. of participants |
9,421 |
9,421 |
9,421 |
9,421 |
|
|
No. of cases |
609 (1.62) |
549 (1.46) |
579 (1.54) |
515 (1.37) |
|
|
KHEI score |
42.00 [14.89–46.92] |
50.69 [46.92–54.01] |
57.29 [54.01–61.01] |
65.89 [61.01–88.00] |
|
|
Model 1 |
ref |
0.88 (0.78–0.98) |
0.91 (0.81–1.02) |
0.79 (0.70–0.89) |
< 0.001 |
|
Model 2 |
ref |
0.88 (0.78–1.00) |
0.93 (0.82–1.05) |
0.83 (0.73–0.95) |
0.016 |
|
Model 3 |
ref |
0.89 (0.78–1.01) |
0.92 (0.81–1.05) |
0.82 (0.71–0.93) |
0.007 |
|
Men (n = 18,316) |
|
|
|
|
|
|
No. of participants |
4,579 |
4,579 |
4,579 |
4,579 |
|
|
No. of cases |
442 (2.41) |
460 (2.51) |
440 (2.40) |
434 (2.37) |
|
|
KHEI score |
38.51 [15.57–43.08] |
46.84 [43.08–50.16] |
53.50 [50.16–57.33] |
62.24 [57.33–85.10] |
|
|
Model 1 |
ref |
1.07 (0.94–1.22) |
1.02 (0.89–1.16) |
1.02 (0.89–1.16) |
0.937 |
|
Model 2 |
ref |
1.09 [0.95–1.26] |
1.08 [0.93–1.25] |
1.13 [0.97–1.31] |
0.153 |
|
Model 3 |
ref |
1.07 [0.93–1.23] |
1.08 [0.93–1.24] |
1.11 [0.95–1.29] |
0.209 |
REFERENCES
- 1. International Diabetes Federation. IDF Diabetes Atlas. 11th ed. International Diabetes Federation; 2025.
- 2. Korea Disease Control and Prevention Agency (KDCA). 2022 Chronic disease status and issues. KDCA; 2022.
- 3. Uusitupa M, Khan TA, Viguiliouk E, Kahleova H, Rivellese AA, Hermansen K, et al. Prevention of type 2 diabetes by lifestyle changes: a systematic review and meta-analysis. Nutrients 2019; 11(11): 2611.ArticlePubMedPMC
- 4. Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 2011; 34(6): 1249-1257. ArticlePubMedPMC
- 5. Toi PL, Anothaisintawee T, Chaikledkaew U, Briones JR, Reutrakul S, Thakkinstian A. Preventive role of diet interventions and dietary factors in type 2 diabetes mellitus: an umbrella review. Nutrients 2020; 12(9): 2722.ArticlePubMedPMC
- 6. Yun S, Park S, Yook SM, Kim K, Shim JE, Hwang JY, et al. Development of the Korean Healthy Eating Index for adults, based on the Korea National Health and Nutrition Examination Survey. Nutr Res Pract 2022; 16(2): 233-247. ArticlePubMedLink
- 7. Shin S, Lee S. Relation between the total diet quality based on Korean Healthy Eating Index and the Incidence of metabolic syndrome constituents and metabolic syndrome among a prospective cohort of Korean adults. Korean J Community Nutr 2020; 25(1): 61-70. ArticleLink
- 8. Lee E, Kim JM. The association of the Korean Healthy Eating Index with chronic conditions in middle-aged single-person households. Nutr Res Pract 2023; 17(2): 316-329. ArticlePubMedPMCLink
- 9. Shim JS, Oh K, Jung SJ, Kim HC. Self-reported diet management and adherence to dietary guidelines in Korean adults with hypertension. Korean Circ J 2020; 50(5): 432-440. ArticlePubMedPMCLink
- 10. Park S, Kim K, Lee BK, Ahn J. A healthy diet rich in calcium and vitamin C is inversely associated with metabolic syndrome risk in Korean adults from the KNHANES 2013-2017. Nutrients 2021; 13(4): 1312.ArticlePubMedPMC
- 11. Kim S, Park M. Association between the Korean Healthy Eating Index (KHEI) and healthcare costs among adults: the Korea National Health and Nutrition Examination Survey (KNHANES) 2016 and 2021. Nutrients 2025; 17(13): 2237.ArticlePubMedPMC
- 12. Kautzky-Willer A, Leutner M, Harreiter J. Sex differences in type 2 diabetes. Diabetologia 2023; 66(6): 986-1002. ArticlePubMedPMCPDF
- 13. Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev 2016; 37(3): 278-316. ArticlePubMedPMC
- 14. Yi Y, An J. Sex differences in risk factors for metabolic syndrome in the Korean population. Int J Environ Res Public Health 2020; 17(24): 9513.ArticlePubMedPMC
- 15. Kim SH, Joung H. Association between the Korean Healthy Diet Score and metabolic syndrome: effectiveness and optimal cutoff of the Korean Healthy Diet Score. Nutrients 2024; 16(19): 3395.ArticlePubMedPMC
- 16. Korea Disease Control and Prevention Agency (KDCA). Korean Genome and Epidemiology Study Basic Survey Data Collection. KDCA: 2017.
- 17. Kim Y, Han BG; KoGES group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) consortium. Int J Epidemiol 2017; 46(2): e20. ArticlePubMed
- 18. Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 1986; 124(1): 17-27. ArticlePubMed
- 19. Korea Disease Control and Prevention Agency (KDCA). Korean genome and epidemiology study Research Guidelines (based survey and examination). KDCA: 2011.
- 20. World Health Organization (WHO). The Asia-Pacific perspective: redefining obesity and its treatment. WHO; 2000.
- 21. Korea Disease Control and Prevention Agency (KDCA). Korean Genome and Epidemiology Study nutritional survey guidelines. KDCA; 2011.
- 22. Kim HR. Nutrition transition and shiting diet linked noncommunicable diseases and policy issues. Health Welf Policy Forum 2013; 198: 27-37.
- 23. Ministry of Health and Welfare; The Korean Nutrition Society. Dietary reference intakes for Koreans 2020. Ministry of Health and Welfare; 2020.
- 24. Korean Diabetes Association. Understanding/treatment/management of diabetes [Internet]. Korean Diabetes Association; n.d. [cited 2023 Sep 25]. Available from: https://www.diabetes.or.kr/general/info/info_01.php
- 25. Jeong YH, Park EJ, Jeon JA, Ko SJ, Kim DE, Lee NH, et al. The current status of life-style related diseases and policy directions. Korea Institute for Health and Social Affairs; 2014 Dec. Report No. 연구보고서 2014-09.
- 26. Zeraattalab-Motlagh S, Jayedi A, Shab-Bidar S. Mediterranean dietary pattern and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of prospective cohort studies. Eur J Nutr 2022; 61(4): 1735-1748. ArticlePubMedPDF
- 27. InterAct Consortium. Adherence to predefined dietary patterns and incident type 2 diabetes in European populations: EPIC-InterAct Study. Diabetologia 2014; 57(2): 321-333. ArticlePubMedPDF
- 28. Pastorino S, Richards M, Pierce M, Ambrosini GL. A high-fat, high-glycaemic index, low-fibre dietary pattern is prospectively associated with type 2 diabetes in a British birth cohort. Br J Nutr 2016; 115(9): 1632-1642. ArticlePubMedPMC
- 29. Schulze MB, Hoffmann K, Manson JE, Willett WC, Meigs JB, Weikert C, et al. Dietary pattern, inflammation, and incidence of type 2 diabetes in women. Am J Clin Nutr 2005; 82(3): 675-684; quiz 714-715. ArticlePubMed
- 30. Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Dietary patterns, insulin resistance, and prevalence of the metabolic syndrome in women. Am J Clin Nutr 2007; 85(3): 910-918. ArticlePubMed
- 31. Rashidipour-Fard N, Karimi M, Saraf-Bank S, Baghaei MH, Haghighatdoost F, Azadbakht L. Healthy eating index and cardiovascular risk factors among Iranian elderly individuals. ARYA Atheroscler 2017; 13(2): 56-65. PubMedPMC
- 32. Roshanzamir F, Miraghajani M, Mansourian M, Ghiasvand R, Safavi SM. Association between Healthy Eating Index-2010 and fetuin-a levels in patients with type 2 diabetes: a case-control study. Clin Nutr Res 2017; 6(4): 296-305. ArticlePubMedPMCLink
- 33. Monfort-Pires M, Folchetti LD, Previdelli AN, Siqueira-Catania A, de Barros CR, Ferreira SR. Healthy Eating Index is associated with certain markers of inflammation and insulin resistance but not with lipid profile in individuals at cardiometabolic risk. Appl Physiol Nutr Metab 2014; 39(4): 497-502. ArticlePubMed
- 34. AlEssa HB, Malik VS, Yuan C, Willett WC, Huang T, Hu FB, et al. Dietary patterns and cardiometabolic and endocrine plasma biomarkers in US women. Am J Clin Nutr 2017; 105(2): 432-441. ArticlePubMed
- 35. Gantenbein KV, Kanaka-Gantenbein C. Mediterranean diet as an antioxidant: the impact on metabolic health and overall wellbeing. Nutrients 2021; 13(6): 1951.ArticlePubMedPMC
- 36. Anderson JW, Baird P, Davis RH Jr, Ferreri S, Knudtson M, Koraym A, et al. Health benefits of dietary fiber. Nutr Rev 2009; 67(4): 188-205. ArticlePubMed
- 37. Kim Y, Keogh JB, Clifton PM. Polyphenols and glycemic control. Nutrients 2016; 8(1): 17.ArticlePubMedPMC
- 38. Ye EQ, Chacko SA, Chou EL, Kugizaki M, Liu S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J Nutr 2012; 142(7): 1304-1313. ArticlePubMedPMC
- 39. Tande DL, Magel R, Strand BN. Healthy Eating Index and abdominal obesity. Public Health Nutr 2010; 13(2): 208-214. ArticlePubMed
- 40. Wardle J, Haase AM, Steptoe A, Nillapun M, Jonwutiwes K, Bellisle F. Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med 2004; 27(2): 107-116. ArticlePubMed
- 41. De Paoli M, Zakharia A, Werstuck GH. The role of estrogen in insulin resistance: a review of clinical and preclinical data. Am J Pathol 2021; 191(9): 1490-1498. ArticlePubMed
- 42. Cignarella A, Bolego C. Mechanisms of estrogen protection in diabetes and metabolic disease. Horm Mol Biol Clin Investig 2010; 4(2): 575-580. ArticlePubMed
Citations
Citations to this article as recorded by

 , Minji Kim1),*
, Minji Kim1),* , Kyong Park2),†
, Kyong Park2),†



 KSCN
KSCN
 Cite
Cite


