Regional differences in protein intake and protein sources of Korean older adults and their association with metabolic syndrome using the 2016–2019 Korea National Health and Nutrition Examination Surveys: a cross-sectional study
Article information
Abstract
Objectives
The study aim was to analyze the regional differences in dietary protein intake and protein sources of Korean older adults and their association with metabolic syndrome.
Methods
Study participants were 1,721 older adults aged 65 and over who participated in 2016–2019 Korea National Health and Nutrition Examination Survey. Using 24-hour recall dietary intake data, protein intake and their food sources were examined. The association between protein intake and metabolic syndrome, obesity, and abdominal obesity were analyzed by multiple logistic regression.
Results
Total protein and animal protein intakes were higher in urban area (60.0 g, 24.4 g, respectively) than in rural area (54.6 g, 19.6 g, respectively). With increase of protein intake level, animal to total protein proportion was increased in both areas. Total protein and plant protein intake was negatively associated with the risk of obesity, abdominal obesity in both areas. Animal protein intake was negatively associated with the risk of obesity in both areas, and with abdominal obesity only in urban area. In urban area, plant protein intake was also negatively associated with the risks of metabolic syndrome, elevated triglyceride, and reduced high density lipoprotein-cholesterol. In urban area, the risk of metabolic syndrome was decreased when their protein intake was more than 0.91 g/kg and was lowest when their protein intake was more than 1.5 g/kg (P for trend < 0.001).
Conclusions
Korean older adults showed inadequate protein intake and those in rural area showed lower animal protein intake than in urban area. The risk of obesity and metabolic syndrome was decreased with the increase of protein intake level. These findings may help develop effective nutrition support strategy for older adults to reduce regional health disparity.
INTRODUCTION
Recently, there has been increasing interest in protein intake for the older adults. Protein is involved in normal growth, physiological functions, and life maintenance, and along with carbohydrates and fats, it is 1 of the 3 major energy-providing nutrients, making it an important nutrient for maintaining the health of the older adults [1]. According to the Korea Disease Control and Prevention Agency (KCDC), in 2021, the protein intake of Korean adults was 74 g/day, which was 131.3% of the recommended nutrient intake (RNI) and 16.3% of total energy intake [2]. However, there have been concerns that protein intake of the older adults in Korea could be inadequate considering their low energy intake level, their eating habits based on rice and kimchi, lack of financial ability to purchase high-quality protein foods, and decreased chewing ability. In fact, in a study using data from the Korea National Health and Nutrition Examination Survey (KNHANES) from 2010 to 2019, the proportion of those consuming protein intake lower than Estimated Average Requirement (EAR) among seniors aged 65 or older was found to be 34.5% for men and 44.7% for women, which is higher than that of the young and middle-aged. This report shows that a significant number of Korean older adults have insufficient protein intake, and the quality of protein is also likely to be insufficient [3].
Previous research has reported that increased energy intake from protein can increase satiety, fatty acid oxidation, and lean body mass, as well as lower blood pressure, positively impacting weight control and cardiovascular disease management [4-6]. On the other hand, studies have also reported that high protein intake may have adverse effects on diabetes, cardiovascular disease, cancer, and mortality [7-9]. The associations between plant-based and animal-based protein intake and cardiovascular and metabolic diseases have been reported, but with inconsistent results [10-13]. Additionally, protein deficiency in the older adults has been consistently reported as an important risk factor for frailty and sarcopenia, and efforts have been made to establish protein intake recommendations for the prevention of these conditions [14,15].
Meanwhile, urban and rural areas may have differences in lifestyles and dietary habits due to differences in regional environments [16]. Rural areas tend to have fewer opportunities for nutrition management services compared to urban areas, and food support programs are also less actively implemented, increasing the need for nutrition support in rural areas [17]. Previous studies have shown that the risk of protein deficiency was higher in older adult women living in rural areas compared to those living in urban areas [18], and the dietary quality of rural older adults was lower than that of urban elderly residents [19,20]. Rural older adult residents often consume meals consisting of rice and kimchi, with side dishes primarily composed of vegetables [18,19,21]. And these differences in nutrient intake between urban and rural areas may be related to the incidence of chronic diseases and contribute to health inequalities across regions [22-24].
As the aging population in South Korea is rapidly increasing, there is growing interest in protein intake among the older adult population. While research has been conducted on protein intake levels for sarcopenia prevention [14,15] and socioeconomic factors related to protein intake [18,25], studies on regional differences in protein intake among older adults are lacking. Therefore, to promote the health of the older adults and prevent and manage chronic diseases, it is necessary to develop food and nutrition policies to support adequate protein intake and address regional disparities. This study aims to utilize data from the KNHANES to compare protein intake levels and protein sources among the older adults in South Korea by region, and to investigate the associations between total, plant-based, and animal-based protein intake levels, and metabolic syndrome-related factors across regions.
METHODS
Ethics statement
The 2016 and 2017 KNHANES were exempted from the Institutional Review Board(IRB) review based on Bioethics and Safety Act in 2016 and 2017. The 2018 and 2019 KNHANES were approved and conducted by the IRB of the KCDC (approval No.: 2018-01-03-P-A, 2018-01-03-C-A).
1. Study participants
To exclude the effects of coronavirus disease 2019, this study utilized data from the 2016–2019 KNHANES. Of the 6,691 individuals aged 65 and older who participated in the survey, those without nutrition survey data (n = 638), those with daily total energy intake less than 500 kcal or exceeding 5,000 kcal (n = 97), those with missing values for variables required for analysis (n = 577), those undergoing treatment for hypertension, dyslipidemia, or diabetes (n = 3,508), those who did not fast for 8 hours before the blood test (n = 38), and those with missing values for metabolic syndrome components from the blood test (n = 52) were excluded from the study. Consequently, a total of 1,721 individuals were included as the final study subjects.
2. Sociodemographic characteristics
The sociodemographic variables used in this study were gender, age, household income, education level, smoking, alcohol consumption, and number of days walked. Subjects were classified into 2 age groups: ‘65–74 years’ and ‘75 years and older.’ Household income was categorized into ‘lowest,’ ‘medium-low,’ ‘medium-high,’ and ‘highest’ based on income quartiles. Education level was classified as ‘elementary school or less,’ ‘middle school,’ ‘high school,’ and ‘college or more.’ Health behavior factors included current smoking and current drinking. Physical activity was categorized into ‘less than 2 days/week,’ ‘2–4 days/week,’ and ‘more than 5 days/week’ using the number of days walking for more than 10 minutes per day in a week.
3. Dietary intake
To assess nutrient intake levels, data from the 24-hour dietary recall method were used. Daily intakes of total energy and the 3 major nutrients (g/day) were analyzed, and the proportions of these nutrients in total energy intake were calculated. Additionally, to evaluate the adequacy of protein intake, the ratio of the RNI was analyzed, and the percentage of individuals with intakes below the EAR was analyzed to determine the proportion of individuals with insufficient protein intake.
In the KNHANES, foods were classified into 20 food groups: grains, potatoes and starches, sugars, legumes, nuts and seeds, vegetables, mushrooms, fruits, seaweeds, seasoning, plant oils, and other plant-based foods. Protein intake from these groups was categorized as plant-based protein. Protein intake from meat, eggs, fish and shellfish, milk, animal oils, and other animal-based foods was categorized as animal-based protein. Beverages and alcoholic drinks were excluded.
To analyze the association between protein intake and obesity and metabolic syndromerelated factors by region, daily protein intake per unit body weight (g/kg/day) was calculated. Based on the EAR (0.73 g/kg), RNI (0.91 g/kg) for 2020 Dietary Reference Intakes for Koreans, and studies by Jung et al. [14] and Park et al. [15] on the relationship between protein intake and sarcopenia, protein intake was classified into 5 groups: ‘less than 0.73 g,’ ‘0.73– 0.91 g,’ ‘0.91–1.2 g,’ ‘1.2–1.5 g,’ and ‘1.5 g or more’ per kg of body weight. Additionally, the association between plant-based and animal-based protein intake and obesity and metabolic syndrome was analyzed. Since there are no separate recommendations for plant-based and animal-based proteins, intake levels were divided into quartiles for analysis.
4. Obesity and metabolic syndrome-related factors
To analyze obesity and metabolic syndrome-related factors, this study utilized waist circumference, systolic and diastolic blood pressure, fasting blood glucose, triglyceride (TG), high-density lipoprotein (HDL) cholesterol, and body mass index (BMI) from the examination survey data of the KNHANES. Physical measurements and biochemical tests were performed by trained personnel following standardized protocols. The diagnosis of metabolic syndrome was based on the definition of the National Cholesterol Education Program Adult Treatment Panel III [26], and the criteria for abdominal obesity were adopted from the Korean Society for the Study of Obesity, considering ethnic differences [27]. Abdominal obesity was defined as a waist circumference of 90 cm or more for men and 85 cm or more for women. Hypertension was defined as a systolic blood pressure of 130 mmHg or higher or a diastolic blood pressure of 85 mmHg or higher. High blood glucose was defined as a fasting blood glucose level of 100 mg/dL or higher. High TG was defined as 150 mg/dL or higher. Low HDL cholesterol was defined as less than 40 mg/dL for men and less than 50 mg/dL for women. Metabolic syndrome was defined as meeting 3 or more of these 5 criteria. Additionally, obesity was defined as a BMI of 25.0 kg/m2 or higher.
5. Statistical analysis
Data processing and analysis were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). All analyses accounted for the complex sample design of the KNHANES, including stratification variables, cluster variables, and weights. The primary comparison was based on residential area, with 'dong' units classified as 'urban areas' and 'eup/myeon' units classified as 'rural areas.' For categorical variables, frequencies and percentages were presented, and for continuous variables, means and standard errors were calculated. The chi-square test or analysis of covariance was conducted to examine differences by region. When comparing the intakes of the 3 major nutrients and plant-based and animal-based protein sources by region, age, gender, and energy intake were adjusted for. To evaluate the association between protein intake levels and obesity and metabolic syndrome factors by region, multiple logistic regression analysis was performed, adjusting for age, gender, household income, education level, smoking status, alcohol consumption, physical activity, and energy intake. Odds ratios (ORs), 95% confidence intervals (CIs), and P for trend were calculated. The level of statistical significance was set at P-value < 0.05.
RESULTS
1. Participant characteristics by region
Table 1 presents a comparison of subject characteristics by region. Approximately 26.8% of the study subjects resided in rural areas. When comparing the characteristics of older adults in urban and rural areas, those living in rural areas had a higher proportion of individuals aged 75 and older, lower income and education levels, higher rates of current smoking, and a higher proportion engaging in walking less than twice a week compared to their urban counterparts. However, there was no regional difference in the rate of current alcohol consumption.
2. Energy and macronutrient intake by region
When comparing energy and macronutrient intake by region (Table 2), urban older adults showed higher intakes of protein and fat compared to those in rural areas. The proportion of total energy from protein was 13.9%, from animal protein was 5.5%, and from fat was 15.9% among urban older adults, which were higher than those of rural older adults, while the proportion of energy from carbohydrates was lower. The ratio of protein intake to the RNI was 108.4% for urban older adults, which was higher than 98.8% for rural older adults. The proportion of individuals with protein intake below the EAR was 40.2% for rural older adults, higher than 33.1% for urban older adults.
3. Protein intake by food group and region
Table 3 shows protein intake by food group and region. The proportion of protein intake from plant sources was higher at 69.0% for rural older adults, while the proportion from animal sources was higher at 36.4% for urban older adults. The food group with the highest protein intake was grains for both urban and rural areas, followed by meat and fish/shellfish. The major plant-based protein sources were grains, vegetables, and legumes, while the major animal-based protein sources were meat, fish/shellfish, eggs, and milk for urban residents, and fish/shellfish, meat, eggs, and milk for rural residents. When analyzing protein intake from each food group, urban older adults showed higher intakes from potatoes/starches, nuts/seeds, mushrooms, eggs, and milk compared to rural older adults. Although not statistically significant, protein intake from meat tended to be higher among urban older adults, while protein intake from grains was higher among rural older adults.
4. Association between protein intake level and energy, macronutrient intake, and metabolic syndrome-related factors by region
Table 4 presents the distribution of protein intake per body weight and the association with energy, macronutrient intake, and metabolic syndrome-related factors by protein intake level and region among Korean older adults. The proportion of individuals meeting the RNI of 0.91 g/kg was 52.3% in urban areas and 45.0% in rural areas, while the proportion consuming 1.2 g/kg or more was 27.6% for urban older adults and 23.2% for rural older adults. As total protein intake increased, animal to total protein proportion increased in both urban and rural areas. Additionally, as protein intake increased, total energy intake, the proportion of energy from protein, and the proportion of energy from fat increased, while the proportion of energy from carbohydrates decreased in both urban and rural older adults.
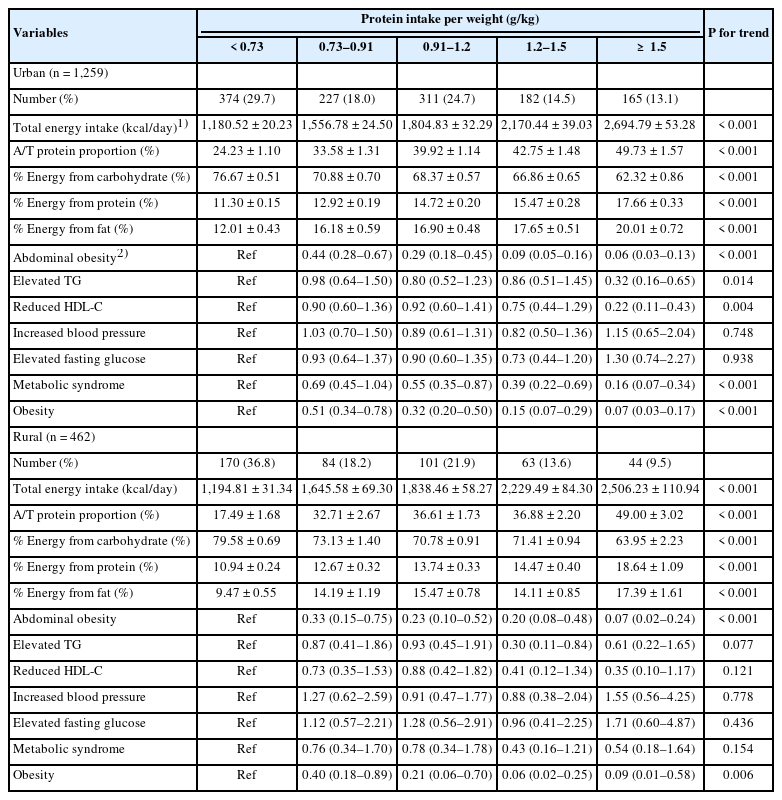
Energy and macronutrient intake, ORs and 95% CIs for obesity and metabolic syndrome parameters according to protein intake per weight of Korean older adults by region
When examining the association between protein intake level and obesity and metabolic syndrome factors by region, higher protein intake was significantly associated with lower ORs for abdominal obesity (P for trend < 0.001), hypertriglyceridemia (P for trend = 0.014), hypo-HDL cholesterolemia (P for trend = 0.004), metabolic syndrome (P for trend < 0.001), and obesity (P for trend < 0.001) among urban older adults. Particularly for hypertriglyceridemia and hypo-HDL cholesterolemia, the ORs were 68% and 78% lower, respectively, when protein intake was 1.5 g/kg/day or higher compared to intake below the EAR. For metabolic syndrome, the OR started decreasing when protein intake was at or above the RNI, and an 84% decrease was observed at an intake of 1.5 g/kg/day or higher. Among rural older adults, higher protein intake was significantly associated with lower OR for abdominal obesity (P for trend < 0.001) and obesity (P for trend = 0.006). In contrast to urban older adults, there were no significant differences in the OR for hypertriglyceridemia, hypo-HDL cholesterolemia, and metabolic syndrome according to protein intake levels. However, the group with a protein intake of 1.2–1.5 g/kg/day had a 70% lower OR for hypertriglyceridemia (OR, 0.30; 95% CI, 0.11–0.84) compared to the group with intake below the EAR.
Figure 1 shows the prevalence of obesity and metabolic syndrome-related factors by protein intake level and region. For urban older adults, higher protein intake was associated with lower prevalence of abdominal obesity, hypo-HDL cholesterolemia, metabolic syndrome, and obesity. However, in rural areas, only the risk of abdominal obesity significantly decreased with higher protein intake.
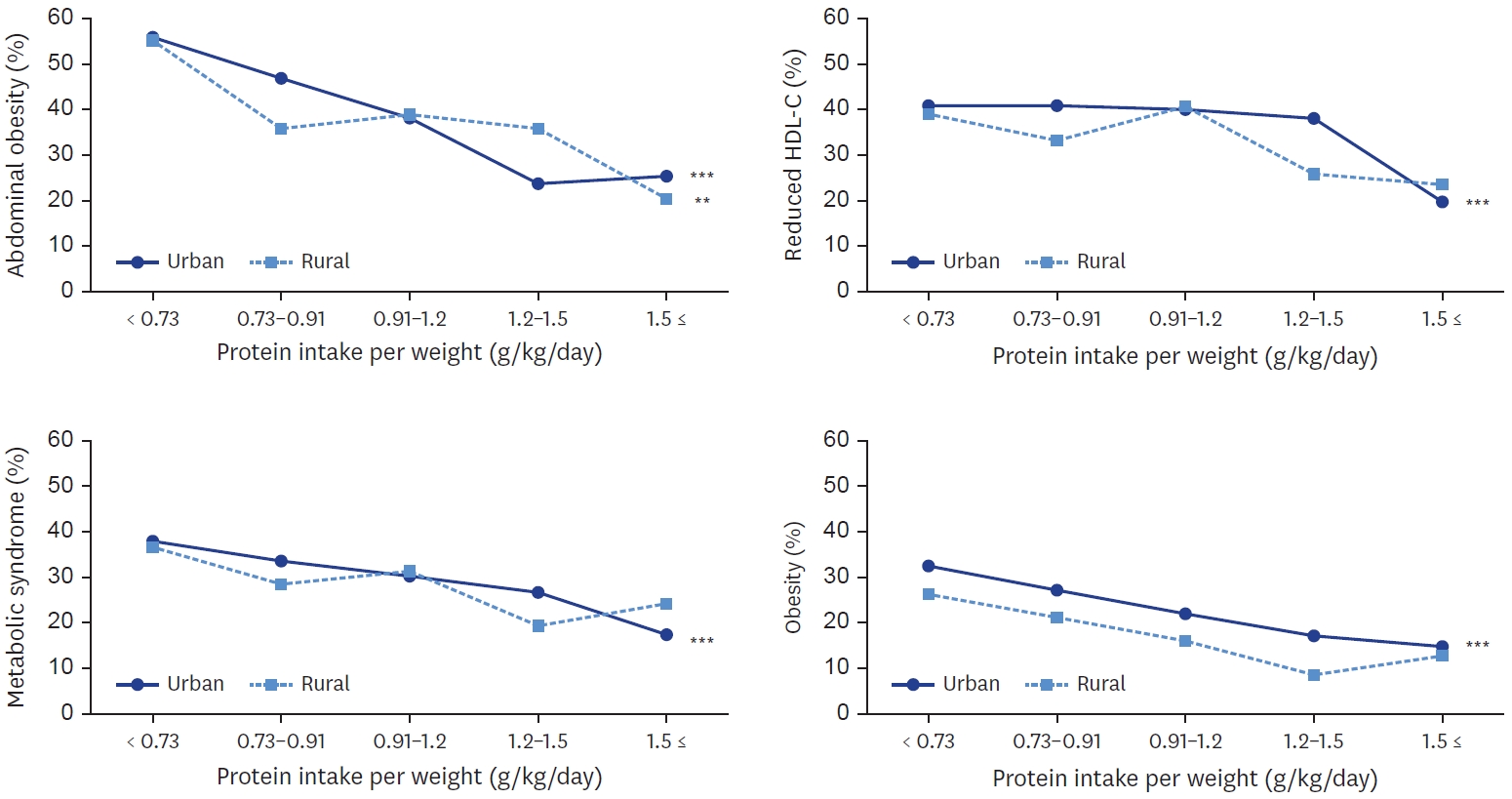
Percentage of obesity, metabolic syndrome, reduced HDL-C and abdominal obesity according to protein intake per weight of Korean older adults by region. All analyses accounted for the complex sampling design effect and appropriate sampling weights. P-value by χ2 test in complex sample survey data analysis. HDL-C, high density lipoprotein-cholesterol.
**P < 0.01, ***P < 0.001.
5. Association between plant-based and animal-based protein intake and obesity and metabolic syndrome factors by region
To investigate whether the association between protein intake and obesity and metabolic syndrome factors differed by protein sources, quartiles of plant-based and animal-based protein intake were analyzed for their association with obesity and metabolic syndrome factors, with the results presented in Table 5. For urban older adults, higher plant-based protein intake was significantly associated with lower ORs for abdominal obesity (P for trend < 0.001), hypertriglyceridemia (P for trend = 0.022), hypo-HDL cholesterolemia (P for trend = 0.001), metabolic syndrome (P for trend < 0.001), and obesity (P for trend < 0.001). Higher animal-based protein intake was significantly associated with lower ORs for abdominal obesity (P for trend = 0.014) and obesity (P for trend = 0.005), but in contrast to plant-based protein intake, there was no association between higher animal-based protein intake and hypertriglyceridemia, hypo-HDL cholesterolemia, or metabolic syndrome risk.
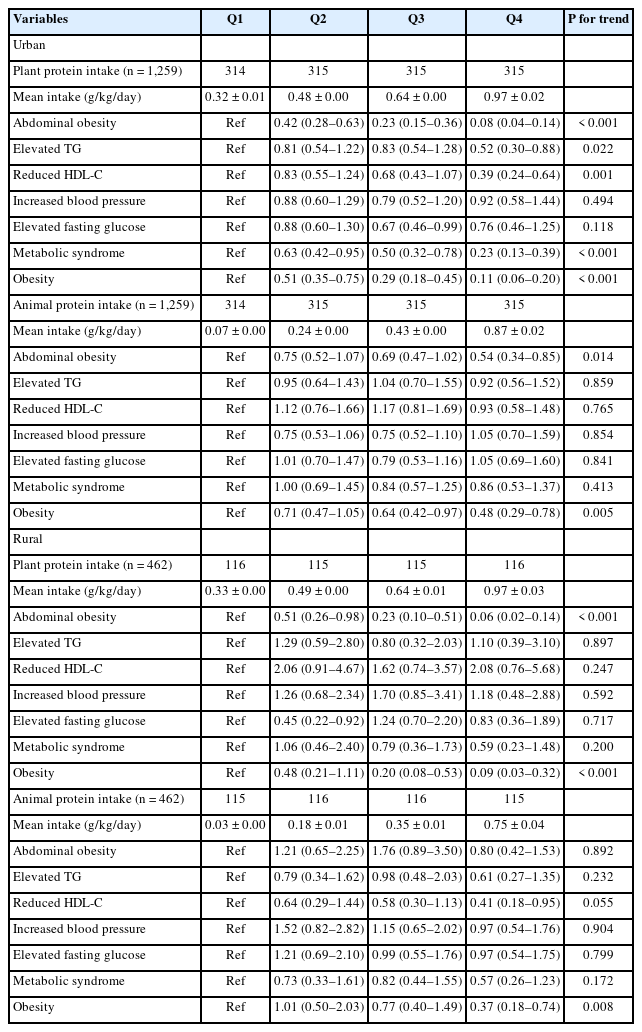
ORs and 95% CIs for obesity and metabolic syndrome parameters according to quartiles of daily plant and animal protein intake per weight of Korean older adults by region
For rural older adults, higher plant-based protein intake was significantly associated with lower ORs for abdominal obesity (P for trend < 0.001) and obesity (P for trend < 0.001). In contrast to urban older adults, there was no association between higher plant-based protein intake and hypertriglyceridemia, hypo-HDL cholesterolemia, or metabolic syndrome risk. However, the second quartile of plant-based protein intake had a 55% lower OR for high fasting glucose (Q2 vs. Q1; OR, 0.45; 95% CI, 0.22–0.92) compared to the lowest quartile. Additionally, higher animal-based protein intake was associated with a lower OR for obesity (P for trend = 0.008), and the highest quartile of animal-based protein intake had a 59% lower OR for hypo-HDL cholesterolemia (Q4 vs. Q1; OR, 0.41; 95% CI, 0.18–0.95) compared to the lowest quartile.
DISCUSSION
This study aimed to compare the differences in protein intake levels and food sources between urban and rural areas among the older adults using data from the 2016–2019 KNHANES. Additionally, it analyzed the association between protein intake levels and the risk of metabolic syndrome by region, identifying protein intake-related factors that contribute to health disparities among the older adult population across regions. The study also aimed to provide basic data for establishing nutrition support programs considering regional characteristics.
In this study, the proportion of older adult individuals aged 75 and older was higher in rural areas compared to urban areas. The differences in population distribution are reported to influence household income and education levels [20,28]. This study also found that household income and education levels were lower among rural older adults compared to their urban counterparts, which is likely to affect dietary habits. Additionally, the intake levels of total protein and animal-based protein were higher among urban older adults than those in rural areas, consistent with findings from previous studies [18,22], indicating regional differences in protein intake. Studies on frailty in the older adults have emphasized the importance of adequate protein intake, as deficiencies in energy, protein, vitamin D, and antioxidant nutrients can contribute to frailty [29,30]. Although consuming sufficient amounts of protein at each meal is crucial for the health of the older adults, many older adults have been reported to have inadequate protein intake [31]. In this study, approximately 35% of the older adults had protein intake below the EAR, with 41% of rural older adults having insufficient intake compared to their urban counterparts. Furthermore, the evaluation of energy contribution from the 3 macronutrients revealed that the proportion of energy from protein and fat was higher among urban older adults, while the proportion from carbohydrates was higher among rural older adults. Although the Korean diet has been changed due to urbanization and Westernization, a high carbohydrate intake, with rice as the staple food, remains a key dietary pattern. Particularly in rural areas, the older adults have been reported to have significantly lower intakes of vegetables (excluding salted vegetables like kimchi), fruits, protein sources, and milk and dairy products [20,32].
When analyzing protein intake by plant-based and animal-based sources, both urban and rural older adults had higher intakes of plant-based protein compared to animal-based protein. However, the proportion of animal-based protein in total protein intake was higher among urban older adults (36.4%), while the proportion of plant-based protein was higher among rural older adults (69.0%). When examining protein intake by food group, rural older adults showed lower intakes from eggs, milk, and a tendency for lower intakes from meat compared to their urban counterparts. This indicates that the lower total protein intake in rural areas is attributable to lower consumption of animal-based protein sources. A prospective cohort study of Americans found that animal-based protein accounted for 60% of total protein intake [12], while Korean older adult individuals, particularly those in rural areas, had a higher reliance on plant-based protein sources.
While various factors influence dietary quality, differences can arise not only due to individual factors such as demographic characteristics, socioeconomic status, and lifestyle but also due to the community food environment [33,34]. Several studies have reported that regional differences in dietary habits can contribute to health inequalities across regions, with older adult individuals in rural areas showing an imbalance in food and nutrient intake compared to their urban counterparts [20,21,28]. An analysis by the Narasalim Research Institute in 2021 found that out of 398 senior welfare centers nationwide, 36.4% were located in Seoul and Gyeonggi Province, while 38 municipalities did not have any senior welfare centers. Additionally, while small scale senior community centers (gyeongrodang) were present in rural area, they lacked systematic programs, indicating regional disparities [35]. Not only are there overall differences in the food environment between urban and rural areas, but the availability of welfare services, such as meal services provided by welfare centers, is likely to have contributed to the regional differences in protein intake among the older adult population. While low protein intake is a widespread issue among the older adults in South Korea, increasing the consumption of protein sources like meat, fish, eggs, beans, milk, and dairy products in rural areas may be challenging through individual efforts alone, suggesting a need for measures to promote a balanced intake across various food groups, including animal-based protein sources [32,36].
In recent years, obesity itself has been classified as a disease, and the prevalence of obesity, metabolic syndrome, diabetes, and other cardiovascular risk factors has shown regional differences [32-34]. In this study, the analysis of the association between protein intake levels and obesity and metabolic syndrome factors revealed that the risk of obesity and abdominal obesity decreased with increasing protein intake in both urban and rural older adult populations, consistent with a previous study by Park et al. [37]. This trend was also observed when analyzing plant-based and animal-based protein intake separately, with the risk of obesity decreasing more substantially with higher plant-based protein intake than with higher animal-based protein intake. Several studies have reported that plant-based protein intake can decrease obesity [38,39], but the effects of animal-based protein intake on obesity have shown conflicting results. A study by Berryman et al. [40] on American adults found that a diet high in animal-based protein had an obesity-reducing effect, while other previous studies on American or Luxembourg adults reported that animal-based protein intake was associated with an increased risk of obesity and abdominal obesity [41,42]. These contradictory results may be related to differences in the distribution of protein intake level among study populations and differences in energy and fat intake levels. In the study by Bujnowski et al. [41], the overall energy and fat intake levels of the study participants were much higher than those in the present study, with the mean animal-based protein intake in the first quartile being 74.7 g and in the fourth quartile being 100.6 g. In contrast, although not presented in the table, the first quartile of animal-based protein intake among the present study participants was only 4.0 g for urban older adults and 1.4 g for rural older adults, while the fourth quartile mean intake was 52.6 g for urban and 43.2 g for rural older adults. In other words, when the study participants have generally higher energy and fat intake and higher protein intake levels, there tends to be a positive correlation between protein intake and obesity. On the other hand, when the overall energy and fat intake of the study participants is relatively low and protein intake is low, a negative relationship could be observed. Park et al. [37] also suggested that there may be a J-curve relationship between animal-based protein intake and obesity. For Korean older adult individuals, not only are their energy and fat intakes generally lower than in previous studies from other countries or Korean adults, but even in the fourth quartile of animal-based protein intake, the intake level is relatively low. Therefore, considering that the protein intake levels of Korean older adults fall on the front part of the J-curve, an increase in protein intake is likely to result in a reduced risk of obesity.
In the analysis of the association between protein intake and metabolic syndrome in this study, urban older adult individuals with protein intake levels at or above the RNI (0.91 g/kg) had a lower risk of metabolic syndrome compared to the group with intake below the EAR (0.73 g/kg), and the risk decreased further with higher protein intake levels. When analyzing plant-based and animal-based protein intake separately, higher plant-based protein intake was associated with a lower risk of metabolic syndrome, while no association was found with animal-based protein intake. A cohort study on Americans reported that higher plant-based protein intake was associated with a slightly decreased risk of overall and cardiovascular disease-related mortality, which is consistent with the trend observed in urban older adult individuals in the present study [12]. However, conflicting results have been reported regarding protein sources. Higher consumption of milk and dairy products has been associated with a decreased risk of metabolic syndrome and its individual components among Korean adults and older adults [43], while a study on Americans found a positive correlation between animal-based protein intake and cardiovascular mortality and a negative correlation with plant-based protein intake [9,13]. While the relationship between protein intake sources and the incidence of cardiovascular disease varies across studies, plant-based protein intake is generally reported to have an inverse relationship with metabolic syndrome and cardiovascular disease.
However, in the present study, no clear association between protein intake and metabolic syndrome was observed among rural older adult individuals. Although a slightly decreasing trend in the prevalence of metabolic syndrome was observed with higher protein intake in rural areas, with the lowest prevalence at a protein intake of 1.2–1.5 g/kg, the difference was not statistically significant, and no significant trend was observed in the OR. The present study alone is limited in explaining why a clear association between protein intake and metabolic syndrome was not observed in rural older adults, unlike in urban areas, and further research is needed. However, when comparing the characteristics of urban and rural older adults within the same protein intake groups, except for the group with the highest intake of 1.5 g/kg, the proportion of animal-based protein intake was remarkably lower in rural areas, and the average proportion of energy from protein in each group was also lower compared to urban areas, while the proportion of energy from carbohydrates was higher. These factors, along with potential differences in overall dietary balance, may have influenced the results.
In this study, urban older adult individuals with a protein intake of 1.5 g/kg or higher showed a significantly lower risk of hypertriglyceridemia and hypo-HDL cholesterolemia, which are components of metabolic syndrome, compared to those with an intake below the EAR (0.73 g/kg). Additionally, this trend was observed only in the highest quartile of plant-based protein intake, and no association was found with animal-based protein intake. In a study by Oh & No [44] on Korean older adults, the group with the highest protein intake (≥ 1.2 g/kg) showed a decrease in hypertriglyceridemia and hypo-HDL cholesterolemia compared to the group with the lowest intake (< 0.8 g/kg). Given the characteristics of Korean older adults having generally low energy, fat, and protein intakes and a high proportion of carbohydrate intake, the energy ratio of carbohydrate:protein:fat in the high protein intake group was analyzed to be more similar to the recommended levels. This dietary pattern is likely to be associated with a reduced risk of obesity, metabolic syndrome, and dyslipidemia.
The diet of Korean older adults is characterized by a very limited variety of foods and high intakes of carbohydrates and sodium. Therefore, increasing protein intake is essential for improving the overall dietary quality of the older adults. The study by Jung et al. [14] recommended a minimum daily protein intake of 1.2 g/kg for the prevention of muscle loss, while Park et al. [15] reported that a 12-week protein supplementation of 1.5 g/kg in frail or pre-frail older adults resulted in increased muscle mass and walking speed compared to those consuming 0.8 g/kg, suggesting the need to increase protein intake in Korean elderly individuals. However, concerns have been raised about the impact of a high-protein diet on the development of kidney disease in the older adults [45,46], and further research is needed to establish protein intake guidelines for this population. Although this study did not analyze the relationship with sarcopenia, the findings demonstrated that increasing protein intake in Korean older adults could have a positive impact on preventing chronic diseases and maintaining health by reducing obesity, abdominal obesity, and metabolic syndrome.
In South Korea, 1 in 3 older adults consume protein below the EAR, indicating a generally low level of protein intake. This situation is particularly pronounced in rural areas, where older adults have lower protein intake levels compared to their urban counterparts and find it challenging to consume a variety of food groups, including protein sources. Despite this, rural areas lack environments that provide balanced meal services through senior welfare centers. Improving meal services in rural areas and in regions with nutritionally vulnerable populations is an urgent task to enhance the intake of both plant-based and animal-based protein sources, given the limited accessibility to protein-rich foods beyond what can be grown in home gardens. In addition to meal services, quantitative and qualitative considerations are needed for food support programs, along with efforts to provide nutrition education and information to the older adults and caregivers to ensure proper utilization of the provided foods.
The limitations of this study are as follows: First, as it is a cross-sectional study, it can only present the association between protein intake and obesity and metabolic syndrome, without establishing a clear causal relationship. Second, the analysis of nutrient intake status was based on data collected through a 24-hour dietary recall, which may not accurately reflect an individual's typical intake. Third, to account for potential dietary changes due to pre-existing conditions, individuals undergoing treatment for hypertension, dyslipidemia, or diabetes were excluded from the study, potentially limiting the characteristics of the study population. Despite these limitations, the strength of this study lies in its use of nationally representative data from the KNHANES to compare protein intake status and sources between urban and rural older adults in South Korea and investigate the association between protein intake and metabolic syndrome-related factors. This study provides baseline data that can be utilized in developing region-specific nutrition support programs for the older adults. Based on the findings, further research is needed to establish appropriate protein intake levels and develop effective protein intake intervention strategies.
CONCLUSIONS
The overall protein intake level of Korean older adults was low, with the intake of total protein and animal-based protein being even lower among rural older adults compared to their urban counterparts. As protein intake increased, the risk of obesity decreased in the older adult population. In urban areas, an increase in plant-based protein intake was significantly associated with a reduced risk of metabolic syndrome. This study is expected to provide foundational information necessary for developing effective nutrition support policies, such as improving foodservice systems, to address regional disparities and ensure adequate nutrient intake among the older adult population.
Notes
Conflict of Interest
There are no financial or other issues that might lead to conflict of interest.
Data Availability
The data that support the findings of this study are openly available in KNHANES at https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do.



